Indice
- 1. Mechanism of action
- 2. Indications
- 3. Metabolism and absorption
- 4. Dosage and drug interactions
- 5. Adverse reactions
- 6. Contraindications
- 7. Laboratory tests
- 8. Conclusions
EDOXABAN
Anticoagulanti Orali Diretti
Edoxaban is an oral direct and reversible inhibitor of activated factor (FXa). It binds to both free and clot bound FXa. Edoxaban is rapidly absorbed, reaching peak plasma concentrations in 1-2 hours with a mean half-life of 8-10 hours in healthy subjects and an oral bioavailability of 50%. It has been approved in Japan for the prevention of venous thromboembolism (VTE) in patients undergoing a total knee arthroplasty, a total hip arthroplasty, and a hip fracture surgery. In September 2014 Edoxaban has been approved in Japan for the prevention of stroke and systemic embolism in patients with non valvular atrial fibrillation (NVAF) and for the treatment and recurrence prevention of deep vein thrombosis (DVT) and pulmonary thromboembolism (PE). In February 2015, edoxaban has been approved by FDA for the treatment of patients with Non Valvular Atrial Fibrillation (NVAF) who had a prior stroke (ischemic or unknown type), transient ischemic attack (TIA) or non-CNS systemic embolism or 2 or more of the following risk factors : a) age > / = 75 years, b) hypertension, c) heart failure, d) diabetes mellitus. The dosage recommended is 60 mg. once daily. The dosage must be reduced at 30 mg. once daily in patients with a creatinine clearance (CrCl) 15 to 50 ml/min, with a low body weight < / = 60 kg or concomitant use of specific P-gp inhibitors such as verapamil, quinidine, dronedarone. Patients on antiretroviral therapy (ritonavir, nelfinavir, indinavir, saquinavir) and patients in treatment with cyclosporine were not included in the ENGAGE AF-TIMI 48 study. The FDA has not approved the use of edoxaban in patients with a CrCl > / = 95 ml/min due to an increased risk of ischemic stroke in patients treated with 60 mg. once daily, compared to patients treated with warfarin. In these patients should be used another anticoagulant.In addition, based on the results of the Hokusai study,the FDA has approved the use of edoxaban in the treatment of patients with Deep Vein Thrombosis (DVT) at the dosage of 60 mg. once daily, following 5-10 days of initial therapy with a parenteral anticoagulant. The dosage must be reduced to 30 mg once daily in case of patients with a CrCl 30 to 50 ml/min, with a body weight < / = 60 kg., or concomitant use of specific P-gp inhibitors such as verapamil and quinidine or the short-term concomitant administration of azithromycin, clarithromycin, erythromycin, oral itraconazole or oral ketoconazol. In April 2015 the European Committee for Medicinal Products for Human Use (CHMP) has recommended approval of edoxaban for the prevention of stroke and systemic embolism in adult patients with non-valvular atrial fibrillation (NVAF) with one or more risk factors. The CHMP has also recommended approval of edoxaban for the treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE), and the prevention of recurrent DVT and PE in adults. In June 2015 edoxaban has been approved in Europe for stroke prevention in NONValvular atrial fibrillation and for the treatment and prevention of recurrent DVT and PE. In the STARS J-5 trial, (1) (Abstract) (Blood 2010 vol. 116 : 3320) edoxaban was compared to enoxaparin in the prevention of deep vein thrombosis in the post-operative period after total hip replacement surgery.
In the STARS E-3 trial, (2) (Abstract ) (Pathophysiology of Haemostasis and Thrombosis 2010 vol. 37 : OC297) patients undergoing total knee replacement surgery, were randomized to receive oral edoxaban or subcutaneous enoxaparin.
In the STARS J-4 trial, (3) (Abstract) (Pathophysiology of Haemostasis and Thrombosis 2010 vol. 37: P366) patients undergoing hip fracture surgery, were randomized in a 2:1 ratio to an edoxaban group or an enoxaparin group.
All the clinical results of these three trials were favorable to the use of oral edoxaban that showed efficacy superior to that of subcutaneous enoxaparin.
In the Hokusai-VTE trial, (4) (NEJM 2013 vol. 369 pp. 1406-1415) patients with acute venous thromboembolism, who had initially received heparin,were randomized to receive edoxaban or warfarin for 3 to 12 months. In this trial, edoxaban showed non inferiority to standard therapy, and caused less bleeding events in a broad spectrum of patients with venous thromboembolism. In this double blind noninferiority trial, 4143 patients received heparin-edoxaban and 4149 patients received heparin-warfarin for a total of 8240 patients, 4921 with deep vein thrombosis and 3319 with pulmonary embolism. The time in the therapeutic range (TTR) among patients taking warfarin was 63.5%. In this trial, if we analyze the geographic provenance of the patients, (see "Supplementary Appendix") we can see that 2676 patients, about 30% of patients randomized in the study, were recruited in Belarus, Brazil, China, India, Mexico, Hungary, Russia, Ukraine, Thailand and Turkey. All these patients have not a good Time in the Therapeutic Range (TTR). For this reasons, can we apply the results of this study to west European Countries and to North America? Certainly not, especially if we consider that in these geographic areas, in specialized anticoagulation clinics, the TTR is > 70% and especially if we consider that combining online management with self testing and/or self dosing can improve INR even further, perhaps to 80% of TTR or better. (5) (Circulation 2012 vol. 126 (5) pp. e52-e54) (see section on "Conclusions")
In the ENGAGE AF-TIMI 48 Investigators trial, (6) (NEJM 2013 vol. 369 pp. 2093-2104) patients with moderate to high risk atrial fibrillation were randomized to receive edoxaban or warfarin. In this randomized, double blind, double dummy trial, two once-daily regimens of edoxaban, 60 mg. once daily in the high dose group, and 30 mg. once daily in the low dose group, were compared to warfarin in 21105 patients with moderate to high risk atrial fibrillation. The mean time in the therapeutic range was 64.9%. The conclusion of the authors was that edoxaban was not inferior to warfarin in the prevention of stroke or systemic embolism and was associated with significantly lower rates of bleeding and death from cardiovascular causes. Also in this trial, if we analyze the geographic provenance of the patients, we can see that 6827 patients, about 30% of the patients, were recruited in countries with a poor time in the therapeutic range (TTR) as Brazil, Bulgaria, China, Colombia, Guatemala, Hungary, India, Mexico, Perù, Philippines, Romania, Russia, Serbia, Thailand, Turkey and Ukraina. Other 4042 patients were recruited in Argentina, Croatia, Czech Republic, Poland and Slovakia and also in these countries there is not a widespread presence of specialized anticoagulation clinics and for this, also these countries have a poor time in the therapeutic range. These patients were in total 10869 patients (52%) of 21105 who were recruited and consequently the conclusions of this study cannot be applied to western european countries and north america which have a great number of specialized anticoagulation clinics where all patients in treatment with vitamin K antagonists should be referred. All these trials will be discussed in detail in the sections “Indications” and “ Conclusions”. Edoxaban is renally excreted for 35%, for 62% is eliminated through feces and is a substrate for P- glycoprotein (P-gp), and for this interferes with the inhibitors and inducers of P-gp. (see section on “Dosage and drug interactions”) Also for edoxaban, as for all the other new oral anticoagulants there is not at the moment an antidote commercially available. Just recently a human volunteer study of 80 individuals has been published by New England Journal of Medicine in which is decribed that PER977 (Aripazine), a synthetic small molecule (D-arginine compound) has a broad activity against various old (unfractioned heparin, low molecular weight heparin) and new oral anticoagulants (dabigatran, rivaroxaban, apixaban and edoxaban). (7) (New England Journal of Medicine 2014, vol. 371 pp.2141-2142) (see section on "Adverse reactions"). Andexanet alfa (r-Antidote, PRT064445; Portola Pharmaceuticals) is a truncated form of enzymatically inactive factor Xa, which binds and reverses the anticoagulant action of the factor Xa inhibitors such as rivaroxaban, apixaban and edoxaban. (8) (Recent Patents on Cardiovascular Drug Discovery 2014 vol. 9 pp. 2-10) (see section on "Adverse reactions") A new study funded by Daiichi Sankyo Development LTD. and Daiichi Sankyo Pharma development, the manufacturer of edoxaban, is evaluating edoxaban compared to warfarin in subjects undergoing cardioversion of atrial fibrillation, the ENSURE-AF study. This study, is a prospective, randomized, open-label, blinded end point evaluation parallel group Phase 3b clinical trial which compares edoxaban with enoxaparin/warfarin followed by warfarin alone in subjects undergoing planned electrical cardioversion of non-valvular atrial fibrillation. (9) (American Heart Journal 2015 vol. 169 pp. 597-604.e5) In a study funded by edoxaban manufacturer, investigators found that halving the dose of edoxaban (i.e., to 30 mg daily in the 60 mg group and to 15 mg daily in the 30 mg group) in 5356 patients with creatinine clearance levels of 30 to 50 mL/min, body weight < / = 60 kg, or concomitant medication with potent P-glycoprotein interaction factors associated with risk for excess drug concentration, was possible to optimize benefits of stroke prevention and minimizing risk for bleeding. (10) (The Lancet 2015 vol. 385 (9984) pp. 2288-2295) Despite several large, randomised trials showing that DOACs are non inferior to warfarin at preventing stroke in patients with atrial fibrillation without increasing bleeding, questions about dosing of DOACs in selected patients with atrial fibrillation still remain. (11) (The Lancet 2015 vol. 385 (9984) pp. 2232-2233) (for details,see section on "Adverse reactions") Clinicians must follow patients who start treatment with new target-specific anticoagulants carefully as weight will change, and medication adjustments are necessary in case of important changes of creatinine clearance. "The notion that patients on these new agents do not need close monitoring is misleading". (12) (Journal Watch April 16, 2015)
References :
1 ) Fuji T., Fujita S., Tachibana S. et al. : Efficacy and safety of edoxaban versus enoxaparin for the prevention of venous thromboembolism following total hip arthroplasty : STARS J-V trial [Abstract]. Blood 2010; 116 : 3320
2 ) Fuji T., Wang C-J., Fujita S. et al. : Edoxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty : the STARS E-3 trial [Abstract]. Pathophysiology Haemostasis and Thrombosis 2010; 37 : OC297
3 ) Fujita S., Fuji T., Tachibana S. et al. : Safety and efficacy of edoxaban in patients undergoing hip fracture surgery [Abstract]. Pathophysiology Haemostasis and Thrombosis 2010; 37 : P366
4 ) The Hokusai-VTE Investigators : Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. New England Journal of Medicine 2013; 369 : 1406-1415
5 ) Bussey Henry I., Bussey Marie : Warfarin Management. International Normalized RatioSelf-Testing and Warfarin Self-Dosing. Circulation 2012; 126 : e52-e54
6 ) Giugliano Robert P., Ruff Christian T., Braunwald Eugene et al. : Edoxaban versus warfarin in patients with atrial fibrillation. New England Journal of Medicine 2013; 369 : 2093-2104
7 ) Ansell J.E., Bakhru Sasha H., Grosso Michael et al. : Use of PER977 to reverse the anticoagulant effect of edoxaban. New England Journal of Medicine 2014 vol. 371 pp. 2141-2142
8 ) Gomez-Outes Antonio, Suarez-Gea M.L., Lecumberri Ramon et al. : Specific antidotes in development for reversal of novel anticoagulants : A review. Recent Patenjts on Cardiovascular Drug Discovery 2014; 9 : 2-10
9 ) Lip Gregory Y.H., Merino José, Ezekowitz Michael et al. : A prospective evaluation of edoxaban compared to warfarin in subjects undergoing cardioversion of atrial fibrillation : The EdoxabaN vs. warfarin in subjectS UndeRgoing CardiovErsionb of atrial fibrillation (ENSURE-AF) study. American Heart Journal 2015; 169 : 597-604.e5
10 ) Ruff Christian T., Giugliano Robert P., Braunwald Eugene et al. : Association between edoxaban dose, concentration, anti-Factor Xa activity, and outcomes : an analysis of data from the randomised, double-blind ENGAGE AF-TIMI 48 Trial. The Lancet 2015; 385 (9984) : 2288-2295
11 ) Patel M.R., Washam J.B. : Edoxaban and the need for outcomes-based NOAC dosing. The Lancet 2015; 385 (9984) : 2232-2233
12 ) Gore Joel M. : Use of clinical factors alone in tailoring edoxaban dose in atrial fibrillation.
Journal Watch April 16, 2015 http://www.jwatch.org/na37398/2015/04/16/use-clinical-factors-alone-tailoring-edoxaban-dose-atrial
1. Mechanism of action
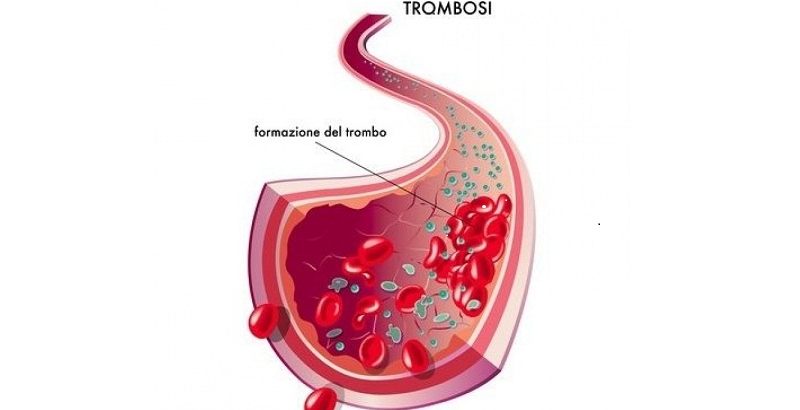
It binds diretly to the catalytic site of factor Xa and inhibits both free and clot bound Xa . Factor Xa , as part of the prothrombinase complex that consists also of factor Va, calcium ions, prothrombin and phospholipids, catalyzes the conversion of prothrombin to thrombin. Thrombin activates platelets, catalyzes the conversion of fibrinogen to fibrin, activates factor V and factor VIII, activates Protein C in the presence of thrombomodulin and Protein S as cofactor, and inhibits fibrinolysis by thrombin activated fibrinolysis inhibitor (TAFI). (see “mechanism of action” of Dabigatran Etexilate review)
References :
1 ) Camm John A., Bounameaux Henri : Edoxaban. Drugs 2011; 71, issue 12 : 1503-1526
2. Indications
In the STARS E-3 trial, a double blind, double dummy trial, 716 patients undergoing a total knee replacement surgery in Japan were randomized to receive oral edoxaban at the dose of 30 mg. once daily or subcutaneous enoxaparin at the dose of 20 mg. twice daily for 10-14 days as prescribed by japanese guidelines.(2) (Abstract) (Pathophysiology of Haemostasis and Thrombosis 2010 vol. 37 : OC297)
The rate of any deep vein thrombosis was 7.4% in the edoxaban group and 13.9% in the enoxaparin group.
The rate of major and clinically relevant nonmajor bleedings were 6.2% in the edoxaban group and 3.7% in the enoxaparin group.
In the STARS J-4 trial, an open label enoxaparin controlled study, 92 patients undergoing hip fracture surgery in Japan, were randomized in a 2 : 1 ratio to edoxaban or enoxaparin.(3) (Abstract) (Pathophysiology of Haemostasis and Thrombosis 2010 vol. 37: P366) The dosages used were the same used in the STARS J-5 trial for elective total hip replacement surgery, and in the STARS E-3 trial for the elective total knee replacement surgery . The rate of thromboembolic events was 6.5% in the edoxaban group and 3.7% in the enoxaparin group. All thromboembolic events were asymptomatic distal deep vein thrombosis. The rate of major and clinically rilevant nonmajor bleedings was 3.4% in the edoxaban group and 6.9% in the enoxaparin group.
All these trials demonstrated a superiority of edoxaban over standard enoxaparin therapy for the less incidence of thromboembolic events, and less major and clinically relevant nonmajor bleedings. In some subgroups of patients with moderate renal impairment (creatinine clearance 30-50 ml/mn), with a body weight < 50 kg. , and/or age = / > 75 years there was a higher bleeding risk with a dosage of edoxaban of 30 mg. once daily and for this, in these particular categories of patients, is recommended a daily dose of 15 mg. A critical revision of these trials will be discussed in the section “Conclusions”.
In the HOKUSAI-VTE trial, a double blind non inferiority trial, 4921 patients with deep vein thrombosis and 3319 patients with a pulmonary embolism who had initially received heparin, were randomized to receive edoxaban at a dose of 60 mg. once daily or 30 mg. once daily in patients with moderate renal insufficiency (creatinine clearance 30-50 ml/mn) or with a body weight < 60 kg., or to receive warfarin. Patients received this treatment for 3 to 12 months. (4) (NEJM 2013 vol. 369 pp. 1406-1415)
Among patients receiving warfarin , the time in the therapeutic range (TTR) was 63.5%. The rate of recurrent symptomatic venous thromboembolism was 3.2% in the edoxaban group and 3.5% in the warfarin group. In a particular subgroup of 938 patients with pulmonary embolism, as assessed by measurement of N-terminal pro-brain natriuretic peptide levels, the incidence of recurrent venous thromboembolism was 3.3% in the edoxaban group and 6.2% in the warfarin group. The rate of major bleeding was 1.4% in the edoxaban group and 1.6% in the warfarin group. The incidence of first major or clinically nonmajor bleeding was 8.5% in the group treated with edoxaban and in 10.3% in the group treated with warfarin. Clinically relevant nonmajor bleeding occurred in 7.2% of patients in the edoxaban group and in 8.9% of patients in the warfarin group. Among patients treated with a reducted dose of 30 mg. of edoxaban once daily, clinically relevant bleeding occurred in 7.9% of patients treated with edoxaban, and in patients treated with warfarin, clinically relevant bleeding occurred in 12.8% of patients. Again in this group, major bleeding occurred in 1.5% of patients in the edoxaban group, and in 3.1% of patients in the warfarin group. Death from any cause occurred in 3.2% of patients in the edoxaban group, and in 3.1% of patients in the warfarin group. Recurrent venous thromboembolism (VTE) and all cause mortality occurred in 5.5% in the edoxaban group and in 5.5% in the warfarin group. The net clinical benefit, venous thromboembolism + major bleeding, was 2.9% in the edoxaban group and 3.5% in the warfarin group.
In the ENGAGE AF-TIMI 48 trial, a randomized, double blind, double dummy trial, two once-daily regimens of edoxaban were compared to warfarin in 21105 patients with moderate to high risk atrial fibrillation. (5) (NEJM 2013 vol. 369 pp. 2093-2104)
As described in the apixaban review, in a double dummy trial, there are usually two placebos. This is necessary when the drugs are administered by different routes (for example by injection as enoxaparin or by pill as edoxaban) or by different protocol (once daily versus weekly dosing) or to not allow participants to know in which treatment arm they are. In this last case, they usually take one active drug and one of placebo. In fact in this study, each patient received two sets of study drugs : either active edoxaban and a placebo matching warfarin, or a placebo matching edoxaban and active warfarin. The high dose edoxaban group received 60 mg. once daily, and the low dose group received 30 mg. once daily. For patients in each group, the dose was halved if at the time of randomization or if during the study, any of the following characteristics were present : moderate renal impairment (creatinine clearance 30-50 ml/mn), a body weight of 60 kg. or less, or the concomitant use of strong inhibitors of P-glycoprotein, as quinidine, verapamil, dronedarone. In the warfarin group, the median time in the therapeutic range was 68.4% and the mean time in the therapeutic range was 64.9. (The median is the numerical value separating the higher half of a data sample from the lower half). In a modified intention to treat population in the treatment period, stroke or systemic embolism occurred in 1.50% patients per year in the warfarin group and in 1.18% patients per year in the high dose edoxaban group and in 1.61% patients per year in the low dose edoxaban group.
In an intention to treat population in the overall study period, stroke or systemic embolism occurred in 1.80% patients per year in the warfarin group and in 1.57% patients per year in the high dose edoxaban group and in 2.04% patients per year in the low dose edoxaban group. Hemorragic stroke occurred in 0.47% patients per year in the warfarin group, in 0.26% patients in the high dose edoxaban group and in 0.16% patients per year in the low dose edoxaban group. Ischemic stroke occurred in 1.25% patients per year in the warfarin group, in 1.25% patients in the high dose edoxaban group and in 1.77% patients per year in the low dose edoxaban group. Non disabling and non fatal stroke occurred in 1.01% patients per year in the warfarin group, in 0.81% patients in the high dose edoxaban group and in 1.13% patients per year in the low dose edoxaban group. Disabling or fatal stroke occurred in 0.71% patients per year in the warfarin group, in 0.69% in the high dose edoxaban group and in 0.80% in the low dose edoxaban group.
Fatal stroke occurred in 0.45% patients per year in the warfarin group, in 0.42% patients per year in the high dose edoxaban group and in 0.38% patients per year in the low dose edoxaban group. Fatal intracranial bleeding occurred in 0.27% patients per year in the warfarin group, in 0.15% patients per year in the high dose edoxaban group and in 0.08% patients per year in the low dose edoxaban group. Major bleeding occurred in 3.43% patients per year with warfarin, in 2.75% patients per year in the high dose edoxaban group and in 1.61% patients per year in the low dose group. The rates of life threatening bleeding, intracranial bleeding, and major bleeding clinically relevant plus nonmajor bleeding were 0.78% patients per year, 0.85% and 13.02% respectively, with warfarin, as compared with 0.40% patients per year, 0.39%, and 11.10%, respectively with high dose edoxaban and 0.25% patients per year, 0.26% and 7.97%, respectively, with low dose edoxaban. The rate of major gastrointestinal bleeding was 1.51% patients per year with high dose edoxaban, 1.23% with warfarin and 0.82% with low dose edoxaban. The conclusion of the study were that once-daily therapy with edoxaban at either of two dosages was noninferior to warfarin for preventing stroke or systemic embolism in nonvalvular atrial fibrillation patients. Both edoxaban daily dosages, 60 mg and 30 mg, were associated with significantly less major bleeding than warfarin in the trial. Also these last two clinical trials present some limitations that will be discussed in the section "Conclusions".
Edoxaban has been approved in Japan for the prevention of venous thromboembolism (VTE) in patients undergoing a total knee arthroplasty, a total hip arthroplasty, and a hip fracture surgery. In September 2014, Edoxaban has been approved also in Japan for the prevention of stroke and systemic embolism in patients with nonvalvular atrial fibrillation (NVAF) and for the treatment and recurrence prevention of deep vein thrombosis (DVT) and pulmonary embolism (PE) . In October 2014, FDA panel members analyzed data from the ENGAGE AF-TIMI 48 trial, and found that an analysis stratified by renal function showed that patients with a creatinine clearance >/= 80 mL/min did not fare as well on treatment as those with abnormal renal function. Regarding the primary efficacy endpoint which was the time to the first adjudicated stroke, ischemic or hemorrhagic, or systemic embolic event, individuals with a creatinine clearance >/= 80 mL/min fared significantly worse when treated with the 30 mg dose of edoxaban. In patients treated with the 60 mg dose, the results showed the same pattern. Overall the hazard ratio for the primary end point versus warfarin was 1.41 (95% Cl 0.97-2.05) for individuals with normal renal function treated with 60 mg of edoxaban. Probably, because 50 to 60% of edoxaban is excreted by the kidneys, individuals with normal renal function were more likely to be underexposed to treatment. While the panel clearly supported edoxaban's approval, panel members discussed adjusting the dose in future trials based on renal function or limiting the indication to patients with impaired renal function. (6) (www.medscape.com/viewarticle/834164) In February 2015, edoxaban has been approved by FDA for the treatment of patients with Non Valvular Atrial Fibrillation (NVAF) who had a prior stroke (ischemic or unknown type), transient ischemic attack (TIA) or non-CNS systemic embolism or 2 or more of the following risk factors : a) age > / = 75 years, b) hypertension, c) heart failure, d) diabetes mellitus. The dosage recommended is 60 mg. once daily. The dosage must be reduced at 30 mg. once daily in patients with a creatinine clearance (CrCl) 15 to 50 ml/mn, with a low body weight < / = 60 kg or concomitant use of specific P-gp inhibitors such as verapamil, quinidine, dronedarone. Patients on antiretroviral therapy (ritonavir, nelfinavir, indinavir, saquinavir) and patients in treatment with cyclosporine were not included in the ENGAGE AF-TIME 48 study. The FDA has not approved the use of edoxaban in patients with a CrCl > / = 95 ml/min due to an increased risk of ischemic stroke in patients treated with 60 mg once daily, compared to patients treated with warfarin. In these patients should be used another anticoagulant. Based on the results of the Hokusai study, the FDA has approved the use of edoxaban in the treatment of patients with Deep Vein Thrombosis (DVT) at the dosage of 60 mg once daily, following 5-10 days of initial therapy with a parenteral anticoagulant. The dosage must be reduced to 30 mg once daily in case of patients with a CrCl 30 to 50 ml/min, with a body weight < / = 60 kg, or concomitant use of specific P-gp inhibitors such as verapamil and quinidine or the short-term concomitant administration of azithromycin, clarithromycin, erythromycin, oral itraconazole or oral ketoconazol. In April 2015, the European Committee for Medicinal Products for Human Use (CHMP) has recommended the approval of edoxaban for the prevention of stroke and systemic embolism in adult patients with non-valvular atrial fibrillation (NVAF) with one or more risk factors. The CHMP has also recommended approval of edoxaban for the treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE), and the prevention of recurrent DVT and PE in adults. In June 2015 edoxaban has been approved in Europe for stroke prevention in Nonvalvular Atrial Fibrillation and for the treatment and prevention of recurrent DVT and PE.
References :
1 ) Fuji T., Fujita S., Tachibana S. et al. : Efficacy and safety of edoxaban versus enoxaparin for the prevention of venous thromboembolism following total hip arthroplasty : STARS J-V trial [Abstract]. Blood 2010; 116 : 3320
2 ) Fuji T., Wang C-J., Fujita S. et al. : Edoxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty : the STARS E-3 trial [Abstract]. Pathophysiology Haemostasis and Thrombosis 2010; 37 : OC297
3 ) Fujita S., Fuji T., Tachibana S. et al. : Safety and efficacy of edoxaban in patients undergoing hip fracture surgery [Abstract]. Pathophysiology Haemostasis and Thrombosis 2010; 37 : P366
4 ) The Hokusai-VTE Investigators : Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. New England Journal of Medicine 2013; 369 : 1406-1415
5 ) Giugliano Robert P., Ruff Christian T., Braunwald Eugene et al. : Edoxaban versus warfarin in patients with atrial fibrillation. New England Journal of Medicine 2013; 369 : 2093-2104
6 ) O' Riordan Michael : FDA advisory panel votes 9 to 1 in favor of edoxaban for stroke prevention in AF patients. www.medscape.com/viewarticle/834164 October 30, 2014
3. Metabolism and absorption
Therefore the unchanged edoxaban detected in the feces was a result of both unabsorbed drug and hepatobiliary excretion of systematically absorbed drug. Unchanged edoxaban is the predominant form in plasma. In a dedicated pharmacokinetic study, total systemic exposures to edoxaban for subjects with CrCl between 50 and 80 ml/mn, CrCl between 30 and 50 ml/mn and CrCl < 30 ml/mn were increased 32%, 72%, 74% respectively relative to subjects with CrCl > / = 80 ml/mn. In a dedicated pharmacokinetic study, patients with mild or moderate hepatic impairment (classified as Child Pugh A or Child Pugh B ) exibited similar pharmacokinetics and pharmacodynamics to their matched healthy control group. Ther is no clinical experience with edoxaban in patients with severe hepatic impairment. (4) (U.S. label 2015) Plasma protein binding of edoxaban is approximately 55%, which is lower than with apixaban (87%) and rivaroxaban (90%). Its relatively low protein binding may be an important property of edoxaban because of implications for patients on hemodialysis treatment; hemodialysis did not affect protein binding, exposure or clearance of edoxaban.(5) (Drugs 2011; 71 issue 12 : 1503-1526)
References :
1 ) Ogata Koichiro, Harary-Mendell Jeanne, Tachibana Masaya et al. : Clinical safety, tolerability, pharmacokinetics, and pharmacodynamics of the novel factor Xa inhibitor edoxaban in healthy volunteers.
The Journal of Clinical Pharmacology 2010; 50, issue 7, : 743-753
2 ) Broadmann M. : Do novel oral anticoagulants do better than standard therapy in the treatment of deep vein thrombosis ? Hamostaseologie 2013; 3 : 218-224
3 ) Mikkaichi Tsuyoshi, Yoshigae Yasushi, Masumoto Hiroshi et al. : Edoxaban transport via P-Glycoprotein is a key factor for the drug's disposition. Drug, Metabolism and Disposition 2014; 42 : 520-528
4 ) U.S.label for Savaysa (Edoxaban)tablet for oral use. www.accessdata.fda.gov/drugsatfda_docs/label/2015/206316lbl
5 ) Camm John A., Bounameaux Henri : Edoxaban. Drugs 2011; 71, issue 12 : 1503-1526
4. Dosage and drug interactions
In patients with a severe renal insufficiency (creatinine clearance < 30 ml/mn), edoxaban was not used.
In the treatment of patients with venous thromboembolism and in patients with pulmonary embolism, edoxaban was administered at a dose of 60 mg. taken with or without food. In patients with a moderate renal impairment (creatinine clearance 30-50 ml/mn), with a body weight of 60 kg. or less and in patients who were in treatment with potent P-glycoprotein inhibitors as verapamil, quinidine , dronedarone and amiodarone, the dosage was reduced to 30 mg. once daily. The treatment was continued for 3 to 12 months.
In the treatment of patients with moderate to high risk atrial fibrillation, edoxaban was used at the dosage of 60 mg. once daily in a group of patients and of 30 mg. once daily in another group of patients with a median follow-up of 2.8 years. The dosage was reduced at 30 mg. and at 15 mg. respectively in the two groups, if at the time of randomization or during the study , were present a moderate renal impairment (creatinine clearance 30-50 ml/mn), a body weight of 60 kg. or less, or the concomitant use of strong P-glycoprotein inhibitors as verapamil, quinidine, dronedarone. In all these categories of patients, it is useful to determine the edoxaban concentration using a calibrated chromogenic anti-Xa assay, after 1-2 weeks when a steady state is obtained.
Drug interactions
Because less than 4% of edoxaban is metabolised by CYP3A4, (1) (Hamostaseologie 2013 vol. 33 pp. 218-224) and because it is a substrate of transport P-glycoprotein, edoxaban, differently from the other factor Xa inhibitors already commercially available, as rivaroxaban and apixaban, interferes only with P-gp inhibitors and with P-gp inducers. With the concomitant use of strong P-gp inhibitors as verapamil, quinidine and dronedarone , it is recommended to halve the dosage normally used in the trials we examined before. On the other hand, this dose reduction was used in all the trials about edoxaban, actually published.
Coadministration of verapamil, quinidine, or dronedarone resulted in > 50% increase in total exposure of edoxaban measured as AUC (area under the curve), and a slight increase in the 24-h concentrations.
Edoxaban coadministered with amiodarone increased total exposure by < 50% measured as AUC ,and by > 50% measured as Cmax, and 24-h concentration decreased by approximately 26%. (2) (American Journal of Cardiovascular Drugs 2013 vol. 13 pp. 331-342) In particular administration of amiodarone causes a 40% increase of edoxaban AUC, Cyclosporine a 73% increase of edoxaban AUC, Dronedarone a 85% increase, Erythromycin a 85% increase, ketoconazole a 87% increase, Quinidine a 76% increase, Verapamil a 53% increase. Other P-gp inhibitors including diltiazepam, itraconazole, clarithromycin, grapefruit jiuce, propafenone, and protease inhibitors such as ritonavir, will increase the AUC of edoxaban. Currently, the manufacturer of edoxaban does not recommend a dose adjustement when P-gp inhibitors are coadministered, even though the increases in edoxaban plasma concentrations may exceed the degree of increase that triggers a dose reduction recommendation in patients with renal dysfunction. (3) (www.pharmacytimes.com August 11,2015) . In patients in treatment with strong P-gp inducers such as carbamazepine, phenytoin, phenobarbital, rifampin, St. John’s Wort and systemic dexamethasone it is better to avoid the use of edoxaban due to the decrease of its AUC. In fact rifampin decreases the AUC of edoxaban by about 35%. In any case, patients stabilized on edoxaban should be monitored for altered response (bleeding or loss of anticoagulant effect) if P-gp inhibitors or inducers are added or removed from their drug regimen. (3) (www.pharmacytimes.com August 11, 2015) In subjects with renal dysfunction (creatinine clearance between 30 and 50 ml/mn), the area under the concentration time curve (AUC) of edoxaban increased 35% to 60%. (4) (Journal of Clinical Pharmacology 2015 vol. 55 (11) pp. 1268-1279)
For conversion from vitamin K antagonists to edoxaban, warfarin or other vitamin K antagonists must be discontinued and start edoxaban when the international normalized ratio (INR) is < 2.0.
For conversion from edoxaban to vitamin K antagonists, because edoxaban affects INR, this test cannot be used during co-administration with warfarin for determining the appropriate dose of warfarin. If continuos anticoagulation is necessary, edoxaban must be discontinued, and start both a parenteral anticoagulant and warfarin at the next scheduled dose of edoxaban, discontinuing the parenteral anticoagulant when the INR reaches an acceptable range.
For conversion from edoxaban to anticoagulants other than vitamin K antagonists, edoxaban must be discontinued, and the other anticoagulant can be started at the next edoxaban scheduled dose. Also in these last two cases, before starting a therapy with another anticoagulant, can be useful to perform a calibrated chromogenic anti-Xa assay.
References :
1 ) Broadmann M. : Do novel oral anticoagulants do better than standard therapy in the treatment of deep vein thrombosis ? Hamostaseologie 2013; 3 : 218-224
2 ) Mendell Jeanne, Zahir Hamim, Matsushima Nobuko et al. : Drug-drug interaction studies of cardiovascular drugs involving P-Glycoprotein, an efflux transporter, on the pharmacokinetics of edoxaban, an oral factor Xa inhibitor. American journal of Cardiovascular Drugs 2013; 13 : 331-342
3 ) Horn John R. and Hansten Philip D. : Edoxaban : A new factor Xa inhibitor anticoagulant. www.pharmacytimes.com
August 11, 2015
4 ) Jonsson S. Simonsson US., Miller R. et al. : Population pharmacokinetics of edoxaban and its main metabolite in a dedicated renal impairment study. Journal of Clinical Pharmacology 2015; 55 (11) : 1268-1279
5. Adverse reactions
Andexanet alfa (PRT064445, r-antidote; Portola Pharmaceuticals) is a modified Factor Xa molecule obtained by recombinant technology that is being developed as antidote for patients receiving a Factor Xa inhibitor who suffer a major bleeding episode or who may require emergency surgery. It is a truncated form of enzymatically inactive factor Xa, which binds and reverses the anticoagulation action of the factor Xa inhibitors such as rivaroxaban, apixaban and edoxaban. It is catalytically inactive and lacks the membrane-binding γ-carboxyglutamic acid domain of native FXa but retains the ability of native FXa to bind directly FXa inhibitors as well as LMWH and fondaparinux-activated antithrombin (AT). Once bound, the FXa inhibitors are unable to bind to and inhibit native FXa, thus allowing for restoration of normal haemostatic processes. (5) (Recent Patents on Cardiovascular Drug Discovery 2014 vol. 9 pp. 2-10) Andexanet alfa dose-dependently reversed the inhibition of FXa by direct FXa inhibitors and corrected the prolongation of ex vivo clotting times by such inhibitors. The effect of andexanet alfa was mediated by sequestering the FXa inhibitor in a 1:1 molar ratio and reducing free fraction and anti-FXa activity of the FXa inhibitor in plasma. (6) (Nature Medicine 2013 vol. 19 (4) pp. 446-451) In a study (7) (Thrombosis and Haemostasis 2012 vol. 107 pp. 253-259) Prothrombin complex concentrates (PCC), Activated Prothrombin complex concentrates (FEIBA) and Recombinant factor VIIa (rFVIIa) significantly reversed the anticoagulant effect of edoxaban in vitro. FEIBA and rVIIa significantly reversed edoxaban-induced prolongation of bleeding time in rats. Because the prothrombotic potential of activated PCCs and rVIIa may be higher than that of non activated PCCs, some guidelines recommend the use of non activated PCCs as the first choice for reversal of the anticoagulant effect of edoxaban and the other new oral anticoagulants. (8) (Thrombosis and Haemostasis 2012 vol. 108 pp. 876-886) Because in 4-factors prothrombin complex concentrates (4-PCCs) there is a wide variation in the amount of factors II, VII, IX and X, and protein C and protein S, and because PCCs are dosed on FIX, the actual administered doses of the other components can vary considerably among different PCCs. PCCs also contain different amounts of anticoagulants as heparin and antithrombin. For these reasons, at the moment, in absence of clinical studies, we do not know if the results obtained with a PCC can be obtained with another one, and in the same time,we do not know which components of PCCs are more important in improving hemostasis when we use new direct inhibitors of factor Xa. We can have a clinical reversal of bleeding, without having a correction of laboratory parameters, and this may be due to the relative insensitivity of some laboratory tests to the presence of the anticoagulant. The dosing and the effectiveness of a therapy for reversal of the new oral anticoagulants depend on the level of the anticoagulant present. At the moment no studies have yet examined the effectiveness of any reversal strategy in bleeding human patients. (9) (Thrombosis and Haemostasis 2014 vol. 111 (2) pp. 189-198) Supportive therapies in case of severe hemorrhage, include mechanical compression, surgical compression, surgical hemostasis procedures, and transfusional support. Differently from the other direct FXa inhibitors commercially available as apixaban and rivaroxaban, that have a high plasma protein binding, edoxaban has a protein binding of about 54% (10) (Hamostaseologie 2013 vol. 3 pp. 218-224) and for this, probably, can be partially removed from plasma by dialysis.
In a recent study funded by edoxaban manufacturer, investigators evaluated the clinical effect of dose reduction of edoxaban in patients with atrial fibrillation. Of the 21105 patients randomly assigned to receive warfarin, higher doser edoxaban (60 mg once daily), or lower dose edoxaban (30 mg once daily), edoxaban doses were halved (i.e., to 30 mg daily in the 60 mg group and to 15 mg daily in the 30 mg group) in 5356 patients with creatinine clearance levels of 30 to 50 mL/min, body weight < / = 60 kg, or concomitant medication with potent P-glycoprotein interaction factors associated with risk for excess drug concentration. The fourfold range in edoxaban dosing was associated with a threefold gradient of mean trough level of edoxaban. Dose reduction resulted in a decrease in mean drug exposure of 29% and 35% in the higher-dose and lower-dose edoxaban groups, respectively, and a decrease in mean anti-FXa activaty of 25% and 20% respectively. There was a 2.4-fold gradient of mean anti-FXa activity with broad overlap between dose groups. The authors concluded that dose reduction of edoxaban did not alter the efficacy of edoxaban compared with warfarin in the prevention of stroke or systemic embolism, ischemic stroke, or all-cause mortality and achieved similar or improved safety outcomes. (11) (The Lancet, published online on March 10, 2015) Despite several large, randomised trials showing that DOACs are non inferior to warfarin at preventing stroke in patients with atrial fibrillation without increasing bleeding, questions about dosing of DOACs in selected patients with atrial fibrillation still remain. (12) (The Lancet, published online on March 10, 2015)
References :
1 ) Kuroda Yasufumi, Hirayama Chie, Hotoda Hitoshi et al. : Postmarketing safety experience with edoxaban in Japan for thromboprophylaxis following major orthopedic surgery. Vascular Health and Risk Management 2013; 9 : 593-598
2 ) Laulicht Bryan, Bakhru Sasha, Connie Lee et al. : Small molecule antidote for anticoagulants. Circulation 2012; 126 : [Abstract] 11395
3 ) Bakhru Sasha, Laulicht Bryan, Jiang Xuan et al. : A synthetic small molecule which reverses over-dosage and bleeding by the new oral anticoagulants. Circulation 2012; 126 : [Abstract] 18809
4 ) Ansell Jack E., Bakhru Sasha H., Grosso Michael et al. : Use of PER977 to reverse the anticoagulant effect of edoxaban. New England Journal of Medicine 2014, 371 : 2141-2142
5 ) Gomez-Outes Antonio, Suarez-Gea M.L., Lecumberri Ramon et al. : Specific antidotes in development for reversal of novel anticoagulants : A review. Recent Patents on Cardiovascular Drug Discovery 2014; 9 : 2-10
6 ) Lu G., De Guzman F.R., Hollenbach S.J. et al. : A specific antidote for reversal of anticoagulation by direct and indirect inhibitors of coagulation factor Xa. Nature Medicine 2013; 19 (4) : 446-451
7 ) Fukuda T., Honda Y., Kamisato C. et al. : Reversal of anticoagulant effects of edoxaban, an oral, direct factor Xa inhibitor, with haemostatic agents. Thrombosis and Haemostasis 2012; 107 (2) : 253-259
8 ) Turpie A.G.G., Kreutz R., Llau J. et al. : Management consensus guidance for the use of rivaroxaban – an oral, direct factor Xa inhibitor. Thrombosis and Haemostasis 2012; 108 (5) : 876-886
9 ) Dickneite G., Hoffman M. et al. : Reversing the new era oral anticoagulants with prothrombin complex concentrates (PCCs) : what is the evidence ? Thrombosis and Haemostasis 2014; 111 (2) : 189-198
10 ) Brodmann M. : Do novel oral anticoagulants do better than standard therapy in the treatment of deep vein thrombosis ? Hamostaseologie 2013; 3 : 218-224
11 ) Ruff Christian T., Giugliano Robert P., Braunwald Eugene et al. : Association between edoxaban dose, concentration, anti-Factor Xa activity, and outcomes : an analysis of data from the randomised, double-blind ENGAGE AF-TIMI 48 trial. The Lancet, published online on March 10, 2015 http://dx.doi.org/10.1016/S0140-6736(14)61943-7
12 ) Patel Manesh R., Washam Jeffrey B. : Edoxaban and the need for outcomes-based NOAC dosing. The Lancet published online on March 10, 2015 http://dx.doi.org/10.1016/S0140-6736(14)62289-3
6. Contraindications
b ) Use of edoxaban in patients with a severe hypertension not well controlled must be avoided
c ) Use of edoxaban in patients with hepatic disease associated with coagulopathy and clinically relevant bleeding risk is contraindicated
d ) Use of edoxaban is contraindicated in patients at increased risk of bleeding as patients with congenital or acquired bleeding disorders, with current or recent gastrointestinal ulceration, recent puncture of large vessels or organ biopsy, recent major emorrhages, (intracranial, gastrointestinal, intraocular, pulmonary) recent major surgery, recent stroke, known or suspected oesophageal varices, arteriovenous malformations, arterial aneurysm, concomitant use of drugs that affect hemostasis (Unfractioned Heparin (UHF), low molecular weight heparins (LMWH), Heparin derivatives, (Fondaparinux), except when we switch to or from edoxaban.
e ) Use of edoxaban in patients in treatment with azole-antimycotics as ketoconazole, itraconazole posaconazole or HIV protease inhibitors as ritonavir is contraindicated, because these drugs are strong inhibitors of P-glycoprotein (P-gp) and because edoxaban is a substrate of P-gp. In case of concomitant use of edoxaban with other inhibitors of P-gp as quinidine, verapamil, dronedarone and eventually with amiodarone, the dose of edoxaban must be halved. (see section on “Dosage and drug interactions”) In these cases edoxaban plasma concentrations increase, and can cause important bleeding. Use in patients who are in treatment with strong inducers of P-glycoprotein (P-gp) as carbamazepine, phenytoin, rifampicin, St. John Wort’s, phenobarbital and systemic dexamethasone must be avoided,
because edoxaban plasma concentrations can decrease to a clinically relevant degree, causing an increase of thrombotic risk.
f ) Use of edoxaban is contraindicated in women who are pregnant and, therefore, in women in fertile age, before starting its use, a pregnancy must be excluded.
g ) In case of invasive or surgical procedures, if these procedures cannot be delayed, it is useful to use a calibrated chromogenic anti-Xa assay to evaluate edoxaban concentration, and eventually use PCCs or FEIBA or rVIIa.
h ) In case of procedures at low risk of bleeding, edoxaban must be discontinued at least 24-48 hours prior to elective surgery or invasive procedures. In case of procedures at moderate or high risk bleeding, edoxaban must be discontinued at least 48-72 hours prior to elective surgery or invasive procedures. In any case, before the elective surgery, also after 48-72 hours the edoxaban discontinuation, it is useful to perform a calibrated chromogenic anti-Xa assay to evaluate edoxaban plasma concentration.
i ) Also if in the HOKUSAI-VTE trial (1) (New England Journal of Medicine 2013 vol. 369 pp. 1406-1415) and in the ENGAGE-AF TIMI 48 trial (2) (New England Journal of Medicine 2013 vol. 369 pp. 2093-2104) the dosages of edoxaban were halved in case of age = / > 75 years, of a weight = / < 60 kg., of a moderate renal impairment (creatinine clearance 30-50 ml/mn) , I recommend to monitor these patients by a calibrated chromogenic anti-Xa assay . In any case, in very elderly patients, and in patients with extreme body weight = / < 60 kg. or = / > 110 kg. , I do not recommend to use edoxaban, until we will not gain more clinical experience treating them in controlled clinical trials in the next years.
l ) Use of edoxaban is contraindicated in patients with thrombocytopenia (platelets < 90000 per cubic millimeter)
References :
1 ) The Hokusai-VTE Investigators : Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. New England Journal of Medicine 2013; 369 : 1406-1415
2 ) Giugliano Robert P., Ruff Christian T., Braunwald Eugene et al. : Edoxaban versus warfarin in patients with atrial fibrillation. New England Journal of Medicine 2013; 369 : 2093-2104
7. Laboratory tests
a ) Suspected overdosage due to excessive drug intake or to decreased drug clearance
b ) Unexplained bleeding in patients taking edoxaban
c ) Thrombotic events during the treatment
d ) To assess patients compliance
e ) In patients with moderate renal insufficiency because they have an increase of edoxaban concentration
f ) In case of patients with moderate hepatic impairment
g ) In case of bridging with other anticoagulants
h ) In case of extreme body weight
i ) In elderly patients because of frequent presence of renal insufficiency that can suddendly precipitate in this category of patients for many reasons as dehydration
l ) In patients requiring reversal of anticoagulation because of life-threatening hemorrhage
m ) In patients taking other drugs that increase edoxaban concentration as inhibitors of P-glycoprotein, or that decrease its concentration, as P-gp inducers (see section on “Dosage and drug interactions”)
n ) Before surgical or invasive procedures, to know the residual amount of edoxaban in plasma, after having discontinued this drug
o ) In patients with a stroke, taking edoxaban, we cannot perform a thrombolysis if we do not know if they are or they are not anticoagulated
p ) When chronic anticoagulation is achieved, 1-2 weeks after initiation of anticoagulant therapy
q ) At regular intervals during clinical visits
r ) Soon before and after introducing additional drugs that may interfere with edoxaban plasma concentration
Laboratory results are dependent on when the last dose of drug was taken. Data from a single dose administration study, showed a peak concentration of about 130 ng/ml after 1 hour the administration of 30 mg. of edoxaban, and of about 260 ng/ml after 1 hour the administration of 60 mg. of edoxaban.
After 24 hours the edoxaban concentrations were about the same, 10 ng/ml, with the two dosages of 30 and of 60 mg. (1) (Journal of Clinical Pharmacology 2010 vol. 50 (7) pp. 743-753)
The PT and the APTT are the most used tests to study coagulation in many laboratories. PT is not very sensitive for measuring the anticoagulant effect of edoxaban, because we can have therapeutic doses of edoxaban with a mild prolongation of PT and also the expression in INR does not correct the variation in results, due to differences in sensitivity of edoxaban to various thromboplastin reagents. A direct linear correlation was observed between plasma concentrations of edoxaban and the PT Ratio and INR with all the thromboplastin reagents. The greatest sensitivity was observed with Neoplastin Plus and the lowest with the Innovin. The expression of values in INR does not reduce the variability in response to reagent across edoxaban concentrations. (2) (Thrombosis Research 2012 vol. 129 pp. e77-e82) For this, we can extrapolate the patient’s INR similar to what is done with rivaroxaban. (3) (Journal of Thrombosis and Haemostasis 2011 vol. 9 pp. 226-228) We plot on a double- log paper the PT results of healthy subjects obtained with our thromboplastin on the perpendicula axis( Y axis), and the PT results of Edoxaban plasma on the horizontal axis (X axis). The Edoxaban ISI, is the slope of the orthogonal regression line. The INRedoxaban is calculated in the same manner as for warfarin. (see section on “Laboratory tests” in the Rivaroxaban review)
Edoxaban increased aPTT in a concentration-dependent manner. Linear correlations were observed between edoxaban plasma concentrastions and aPTT ratios in tests performed with 4 different aPTT reagents. Also for aPTT, mild prolongation corresponds to therapeutic concentration of edoxaban.
As for the other direct inhibitors of FXa as Rivaroxaban and Apixaban, all the determinations performed by a chronometric method will be influenced, and also the presence of Lupus Anticoagulant in patients taking edoxaban cannot be evaluated. Edoxaban demonstrated dose dipendent inhibition of FXa activity and its concentrations can be determined by a calibrated anti-FXa assay by the use of chromogenic substrates. This assay must be calibrated with edoxaban calibrators and controls, and the strong correlation between edoxaban levels and anti-Xa activity in a chromogenic assay, make this test, when available, the most suitable test for quantitation of edoxaban and other direct FXa inhibitors. A modified Rotachrom assay (Stago) can be used for evaluation of edoxaban concentrations, but a new specific test for direct FXa inhibitors, the Hyphen BioMed assay, has been modified for direct FXa inhibitors.
(4) (Thrombosis and Haemostasis 2010 vol. 104 (5) pp. 1078-1079) This test is devoid of AT and for this is unaffected by the presence of heparin. This new test for anti-Xa activity will have particular interest if a heparin-edoxaban drug combination is used. (2) (Thrombosis research 2012 vol. 129 pp. e77-e82)
In any case we need to increase our clinical experience with these assays to determine when exactly measurements of anticoagulant effect will be helpful, to define how assay results will influence our clinical decisions, to correlate anticoagulations levels with efficacy and safety. (5) (Journal of Thrombosis and Haemostasis 2013 vol. 11 pp. 245-252)
References :
1 ) Ogata Koichiro, Harary-Mendell Jeanne, Tachibana Masaya et al. : Clinical safety, tolerability, pharmacokinetics, and pharmacodynamics of the novel factor Xa inhibitor edoxaban in healthy volunteers.
The Journal of Clinical Pharmacology 2010; 50, issue 7, : 743-753
2 ) Samama Meyer Michel, Mendell Jeanne, Guinet Cèline et al. : In vitro study of the anticoagulant effects of edoxaban and its effect on thrombin generation in comparison to fondaparinux. Thrombosis Research 2012; 129, issue 4 : e77-e82
3 ) Tripodi A., Chantarangkul V., Guinet C. et al. : The International Normalized Ratio calibrated for rivaroxaban has the potential to normalize prothrombin time results for rivaroxaban-treated patients : results of an in vitro study. Journal of Thrombosis and Haemostasis 2011; 9 : 226-228
4 ) Samama M.M., Amiral J., Guinet C. et al. : An optimised chromogenic assay, specific for measuring direct factor Xa inhibitors (rivaroxaban) in plasma. Thrombosis and Haemostasis 2010; 104 (5) : 1078-1079
5 ) Garcia D., Barrett Y.C., Ramacciotti E. et al. : Laboratory assessment of the anticoagulant effects of the next generation of oral anticoagulants. Journal of Thrombosis and Haemostasis 2012; 11 : 245-252
8. Conclusions
In the HOKUSAI-VTE trial, (2) (NEJM 2013 vol. 369 pp. 1406-1415) (see section on “Indications”) a double blind noninferiority trial, 4143 patients received heparin-edoxaban and 4149 patients received heparin-warfarin for a total of 8240 patients, 4921 with deep vein thrombosis and 3319 with pulmonary embolism. Patients received treatment for 3 to 12 months. The conclusions of the trial were that “edoxaban administered once daily after initial treatment with heparin, was noninferior to high quality standard therapy and caused significantly less bleeding in a broad spectrum of patients with venous thromboembolism, including those with severe pulmonary embolism” The time in the therapeutic range (TTR) among patients receiving warfarin was 63.5%. In this trial, if we analyze the geographic provenance of the patients, (see “Supplementary Appendix”) we can see that 2676 patients, about 30% of patients randomized in the study, were recruited in Belarus, Brazil, China, India, Mexico, Hungary,Russia , Ukraine, Thailand and Turkey . All these countries have not a good Time in the Therapeutic Range (TTR). Other 517 patients were recruited in Argentina, Czech Republic and Poland that have not an optimal TTR. For this reasons, can we apply the results of this study to west European Countries and to North America ? Certainly not, especially if we consider that in these geographic areas the TTR is = / > 70% and especially if we consider that combining online management with self testing and/or self dosing can improve INR even further, perhaps to 80% of the time in the therapeutic range or better. (3) (Circulation 2012 vol. 126 (5) pp. e52-e54) As for the other new oral anticoagulants we cannot use edoxaban in this indication on a large scale in western European Countries and in North America, but only in limited selected cases as we discussed in the previous reviews, in patients who cannot reach the anticoagulation clinic for personal or health problems, in patients who refuse to take a blood test every three, four weeks, in patients who had an intracranial bleeding while they were taking warfarin and after they need to take anticoagulant therapy again, because of the high rate of recurrence as demonstrated by the Italian Collaborative Study CHIRONE (Cerebral Haemorrhage In patients Restarting Oral aNticoagulant thErapy). (4) (Neurology 2014 vol. 82 pp. 1020-1026) At the moment the use of these new oral anticoagulants can be useful only in countries with a poor quality control of anticoagulant therapy with vitamin K antagonists, especially if we consider that a good quality control cannot be a good TTR only, but also a good clinical control, with periodic clinical, laboratory and instrumental examinations and appropriate therapeutic management of important bleeding caused by vitamin K antagonists. Also considering that at the moment we do not have an antidote commercially available in case of bleeding provoked by the new oral anticoagulants, we understand that in the west countries, the strategy is to try to ameliorate our control of anticoagulant therapy with vitamin K antagonists and not to use new oral anticoagulants on a large scale. Just recently, a letter was published by New England Journal of Medicine in November 2014, in which a new molecule, PER977, was designed to inhibit unfractioned and low molecular weight heparin but binds in a similar way to factor Xa inhibitors anf thrombin inhibitors. The observed effect of both edoxaban and PER977 in this study were confirmed by changes in the diameter of fibrin fibers in scanning electron micrographs of clots obtained during clotting time tests. (5) (New England Journal of Medicine 2014 vol. 371 pp. 2141-2142) For details, see section on "Adverse reactions".
In the ENGAGE AF-TIMI 48 trial, (6) ( New England Journal of Medicine 2013 vol. 369 pp. 2093-2104) a randomized, double blind, double dummy trial, two once-daily regimens of edoxaban, 60 mg. once daily in the high dose group, and 30 mg. once daily in the low dose group, were compared to warfarin in 21105 patients with moderate to high risk atrial fibrillation. (see section on “Indications”) The mean time in the therapeutic range was 64.9%. Also in this trial, if we analyze the geographic provenance of the patients we can see that 6827 patients, about 30% of the patients were recruited in countries with a poor Time in the Therapeutic Range (TTR) as Brazil, Bulgaria, China, Colombia, Guatemala, Hungary, India, Mexico, Perù, Philippines, Romania, Russia, Serbia, Thailand,Turkey and Ukraina. Other 4042 patients were recruited in countries without an optimal Time in the Therapeutic Range as Argentina, Croatia, Czech Republic, Poland, Slovakia. These patients were in total 10869 patients (52%) of 21105 who were recruited. Also in this case, I do not think we can apply the results obtained in this trial to western European Countries and North America for the reasons we discussed before, analyzing the results of the HOKUSAI-VTE trial. Randomized, control trials of optimally managed warfarin versus the new oral anticoagulants, Dabigatran Etexilate, Rivaroxaban, Apixaban and Edoxaban are clearly needed. If we analyze the results of ENGAGE-AF TIMI 48 trial, we can see that in a modified intention to treat population in the treatment period, stroke or systemic embolism occurred in 1.50% patients per year in the warfarin group and in 1.18% patients per year in the high dose edoxaban group and in 1.61% patients per year in the low dose edoxaban group, but in an intention to treat population in the overall study period, the difference between warfarin group and high dose edoxaban group decreased and difference between warfarin group and low dose edoxaban group increased. In fact, in this intention to treat population in the overall study, stroke or systemic embolism occurred in 1.80% patients per year in the warfarin group and in 1.57% patients per year in the high dose edoxaban group and in 2.04% patients per year in the low dose edoxaban group. Ischemic stroke occurred in 1.25% patients per year in the warfarin group and in 1.25% patients per year in the high dose edoxaban group and in 1.77% per year in the low dose edoxaban group. Also if hemorrhagic stroke occurred in 90 patients, 0.47% patients per year in the warfarin group, in 49 patients, 0.26% patients per year in the high dose edoxaban group and in 30 patients, 0.16% patients per year in the low dose edoxaban group, and also if nondisabling and non fatal stroke occurred in 190 patients, 1.01% patients per year in the warfarin group, in 154 patients, 0.81% patients per year in the high dose edoxaban group and in 214 patients, 1.13% patients per year in the low dose edoxaban group, the disabling or fatal stroke occurred in 135 patients, 0.71% patients per year in the warfarin group, in 132 patients, 0.69% patients per year in the high dose edoxaban group and in 152 patients, 0.80% patients per year in the low dose edoxaban group, and fatal stroke occurred in 86 patients, 0.45% patients per year in the warfarin group, in 80 patients, 0.42% patients per year in the high dose edoxaban group and in 73 patients, 0.38% patients per year in the low dose edoxaban group.
Analyzing these results we can see that also if with edoxaban there were less hemorrhagic strokes than warfarin, the number of disabling or fatal stroke was about the same in the warfarin and in the high dose edoxaban group, 135 and 132 respectively. In the low dose edoxaban group was 152.
Also the number of fatal stroke was about the same in the warfarin group and in the high dose edoxaban group, 86 and 80 respectively. In the low dose edoxaban group was 73.
Death from cardiovascular disease occurred in 611 patients, 3.17% patients per year in the warfarin group, in 530 patients, 2.74% patients per year in the high dose edoxaban group and in 527 patients, 2.71% patients per year in the low dose edoxaban group. In this case, would be interesting to know the most important causes of cardiovascular death for every group of patients, to better understand these results.
Also if major bleeding occurred in 524 patients, 3.43% patients per year in the warfarin group, in 418 patients, 2.75% patients per year in the high dose edoxaban group and in 254 patients, 1.61% patients per year in the low dose edoxaban group, there were more gastrointestinal bleedings in the high dose edoxaban group. In fact gastrointestinal bleeding occurred in 190 patients, 1.23% patients per year in the warfarin group, in 232 patients, 1.51% patients per year in the high dose edoxaban group and in 129 patients, 0.82% patients per year in the low dose edoxaban group.
Analyzing these last results, although there was a reduction in major bleeding with edoxaban, there was also an increase in gastrointestinal bleeding, a more common event in the elderly. At the moment because there is not an antidote commercially available, to treat a patient who is taking a new oral anticoagulant with a major or life-threatening hemorrhage, or in preparation for emergent major surgery, is challenging also in the best emergency departments. On the contrary, we can reverse a life-threatening hemorrhage in patients taking vitamin K antagonists using Prothrombin Complex Concentrates (PCCs) and Vitamin K.
There is a need for manufacturer independent trials investigating new oral anticoagulants organized by governmental agencies, although these studies will be very expensive. In any case, if we decide to use edoxaban or other direct FXa inhibitors, we need to monitor patients clinically and by a calibrated chromogenic anti-Xa assay, although it is emphasized that the new oral anticoagulants have a predictable pharmacokinetics and pharmacodynamics, and not only in case of bleeding, thrombosis or in case of an urgent or elective surgery.
At the moment these new agents, should not automatically replace warfarin in patients with atrial fibrillation and should not be used as first line therapy in these patients. (7) (Circulation 2012 vol. 125 pp. 165-170)
References :
1 ) Fuji T., Fujita S., Tachibana S. et al. : Efficacy and safety of edoxaban versus enoxaparin for the prevention of venous thromboembolism following total hip arthroplasty : STARS J-V trial [Abstract]. Blood 2010; 116 : 3320
2 ) The Hokusai-VTE Investigators : Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. New England Journal of Medicine 2013; 369:1406-1415
3 ) Bussey Henry I., Bussey Marie : Warfarin Management International Normalized Ratio Self-Testing and Warfarin Self-Dosing. Circulation 2012; 126 : e52-e54
4 ) Poli D., Antonucci E., Dentali F. et al. : Recurrence of ICH after resumption of anticoagulation with vitamin K antagonists : CHIRONE study. Neurology 2014; 82 : 1020-1026
5 ) Ansell Jack E., Bakhru Sasha H., Grosso Michael : Use of PER977 to reverse the anticoagulant effect of edoxaban. New England Journal of Medicine 2014; 371 : 2141-2142
6 ) Giugliano Robert P., Ruff Christian T., Braunwald Eugene et al. : Edoxaban versus warfarin in patients with atrial fibrillation. New England Journal of Medicine 2013;369: 2093-2104
7 ) Ansell Jack : New oral anticoagulants should not be used as first-line agents to prevent thromboembolism in patients with atrial fibrillation. Circulation 2012; 125 : 165-170